The aim of our lab is to generate large animal models of traumatic brain injury (TBI) and test therapies in these models. We focus on knowledge gaps within clinical care in TBI and post-traumatic sequelae. We are dedicated to high-fidelity models to answer some big, unanswered questions in pathologies resulting from TBI. There is no therapy for TBI besides clinical management strategies. Sometimes these basic, unanswered questions are in populations that few people care about, including pediatric victims of abusive head trauma where the brain injury is inflicted by an adult caretaker to a previously healthy infant or toddler. Model building can be slow; in fact, our Hemispheric Hypodensity model, the first model in any species, took several years of systematic problem solving to develop.
The result of our work might change how young children are managed in the PICU after TBI, improve outcomes after TBI, and the creation of new cell-therapies for specific types of TBI. Understanding the pathophysiology of post-traumatic epilepsy might change how children and adults are treated in the ICU to reduce the incidence of post-traumatic epilepsy.
Broadly, our research has 4 aims:
Understand the pathophysiology of severe TBI in infants and toddlers in order to develop successful therapies.
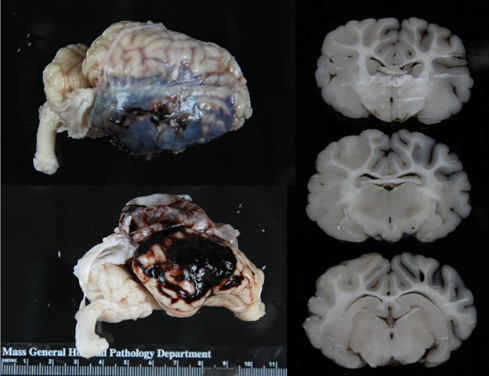
Our model is multi-factorial with the same pathoanatomic injuries and insults observed in young children that develop Hemispheric Hypodensity. The model includes cortical impact, mass effect, subdural and subarachnoid hemorrhage, traumatic seizure, brief apnea, and 10 minutes of hypercapnia. None of these injuries or insults cause wide-spread tissue damage alone, but only when combined.
Hemispheric Hypodensity often occurs from inflicted/abusive head injury though has been observed after an accidental fall from a bunk bed.
Hypoxic-ischemic injury spreads to the cortex at the location of the subarachnoid hemorrhage when seizure occurs for a certain duration of time. The extent and pattern of damage is specific to developmental stage. We are determining if traumatic seizure and subarachnoid drive the pathophysiology of Hemispheric Hypodensity and if stopping seizures with GABA agonists prevents the spread of damage. Worse brain injuries result in more traumatic seizures, but we don’t know yet if traumatic seizures makes the tissue damage worse. We are testing if GABA agonists are a net benefit in the immature brain where GABA is often depolarizing.
Understand the development of the swine brain in relation to the human brain in order to improve the translatability of therapies to children.
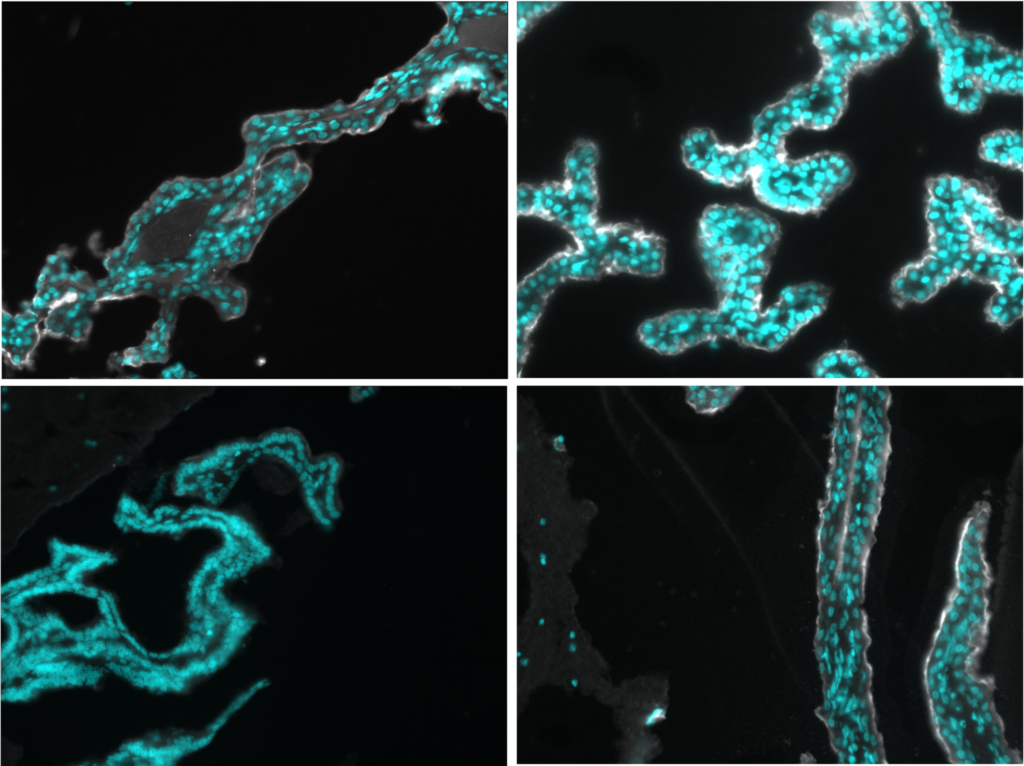
Anatomy, ionic gradients, and inflammatory pathways are species- and development-specific and contribute to differences that developmental stage have on specific pathoanatomic lesions from TBI and might be therapeutic targets to reduce the evolving damage after TBI. Specifically, we describe the anatomy of the subventricular zone and migratory streams, postnatal neuroblast migration and effect of TBI, timing of the GABA switch, chorioid plexus function, and age-dependent up-regulation of matrix metalloproteinases.
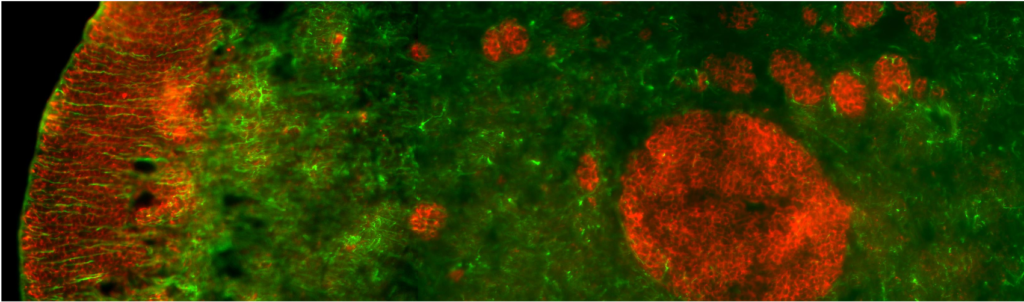
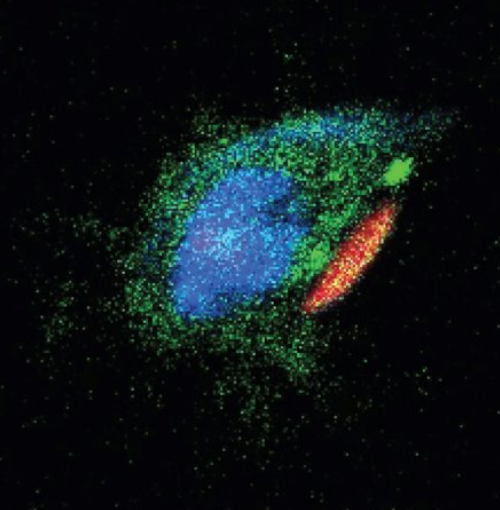
The subventricular zone of the PND 14 piglet (Doublecortin = red)
Serve as a hub of large animal model development, training young scientists while testing novel therapies in order to deploy our models to improve translatability of preclinical TBI research.
We are working on new models of intraventricular hemorrhaged caused hydrocephalus. We demonstrated a positive effect of macrophages engineered to carry therapy-loaded backpacks. We created the first model of epilepsy in swine to understand the pathophysiology and use this model to understand the mechanisms of epileptogenesis and identify biomarkers that might predict the onset of post-traumatic epilepsy.

Create awareness of the the problem of abusive head trauma with the aim of prevention and supporting the medicolegal death investigation system.

This population cannot advocate for themselves. They cannot disclose what happened. The manner in which they were injured is often hidden. The incidence of abusive head trauma is greater than all childhood cancers, yet is relatively unstudied. 80% of moderate to severe TBI in infants is inflicted by a caretaker.
Diagnosis is a multistep process with skeletal surveys, retinal exams, interviews, and genetic screening for potential other causes of hemorrhage or skeletal fractures.
Many parents and pediatricians miss the early signs of abuse which fails to prevent escalation to a severe event. The medicolegal death investigation system is strained with a severe shortage of medical examiners and the resources needed to bring infant homicide victims justice. Often the burden of proof require to prosecute infant homicide cases is greater than required for adult homicide cases.

The MGH Brain Trauma Lab
MGH Neurosciences
Department of Neurosurgery, Massachusetts General Hospital
Department of Neurosurgery, Harvard Medical School